Overview of the Listeria Outbreak
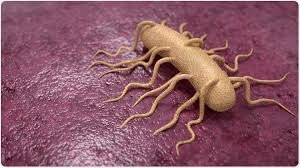
The recent Listeria outbreak in the United States has garnered significant attention due to its severe implications. Listeria monocytogenes, the bacterium responsible for Listeriosis, is typically contracted through the consumption of contaminated food products.
In this case, the source has been traced back to sliced deli meat, a staple in many American diets, thereby increasing the outbreak’s reach and impact.
Listeriosis is particularly dangerous for certain groups of people, including pregnant women, newborns, the elderly, and individuals with weakened immune systems.
The current outbreak has affected multiple states across the country, indicating a widespread distribution of the contaminated meat. As of the latest reports, 28 individuals have been hospitalized, and tragically, two fatalities have been confirmed.
The timeline of the outbreak suggests that the first cases were identified several weeks ago, but the full extent of the contamination is still being investigated.
Health authorities, including the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA), are closely monitoring the situation and providing updates as new information becomes available.
Symptoms, Risks, and Populations Most Affected
Listeria infection, caused by the bacterium Listeria monocytogenes, can present a wide range of symptoms, making it a particularly insidious foodborne illness.
Initially, individuals may experience mild flu-like symptoms such as fever, muscle aches, and gastrointestinal distress, including nausea and diarrhea. However, for certain populations, the infection can escalate to more severe complications.
One of the most alarming aspects of Listeria infection is its potential to cause septicemia and meningitis. Septicemia, or blood poisoning, can lead to systemic inflammation and organ failure.
while meningitis, an infection of the protective membranes covering the brain and spinal cord, can result in neurological damage and even death.
These severe outcomes underline the importance of prompt medical attention if Listeria infection is suspected.
Certain populations are at heightened risk for severe Listeria complications. Pregnant women are particularly vulnerable, as the infection can lead to miscarriage, stillbirth, or premature delivery.
Newborns infected with Listeria can suffer from low birth weight, respiratory distress, and other critical health issues.
Elderly individuals and those with weakened immune systems, such as cancer patients, HIV/AIDS patients, and organ transplant recipients, are also more likely to experience severe disease progression.
The incubation period for Listeria can vary significantly, typically ranging from 1 to 4 weeks after consumption of contaminated food, but cases have been reported with an onset time of up to 70 days. This extended incubation period can complicate the identification and management of the infection.
If individuals suspect they have consumed contaminated deli meat, it is crucial to monitor for symptoms and seek medical advice promptly. Early detection and treatment can significantly improve outcomes.
particularly for those in high-risk groups. Public health advisories and food safety guidelines should be diligently followed to mitigate the risks associated with Listeria outbreaks.
Sources and Distribution of Contaminated Deli Meat
The investigation into the multi-state Listeria outbreak has uncovered significant details about the sources and distribution channels of the contaminated sliced deli meat.
According to the Centers for Disease Control and Prevention (CDC), the outbreak has been traced back to several brands and types of deli meats, including popular varieties such as ham, salami, and turkey breast.
These products were distributed across multiple states, contributing to the widespread nature of the outbreak.
Authorities have identified that the contamination originated at specific processing plants. The plants in question have been linked to numerous suppliers,
leading to the affected deli meats being distributed to various retail locations, including grocery stores and delis, in at least 10 states.
As a result, the contaminated products reached a broad consumer base, increasing the potential for Listeria infections.
Preventative Measures and Public Health Response
Consumers can play a significant role in minimizing their risk of Listeria infection by adhering to safe food handling practices.
Firstly, ensuring that deli meats are properly refrigerated is essential. The ideal refrigerator temperature should be set at or below 40°F (4°C) to inhibit bacterial growth.
Additionally, it is advisable to consume deli meats within three to five days of purchase.
Cooking at the correct temperatures is another preventive measure. For instance, heating deli meats to an internal temperature of 165°F (74°C) can effectively kill Listeria bacteria.
It is also crucial to avoid cross-contamination by using separate cutting boards and utensils for raw and ready-to-eat foods, and washing hands thoroughly before and after handling food.
To prevent future outbreaks, ongoing monitoring and research are essential. Health agencies are continuously updating their recommendations based on the latest scientific findings.
Public awareness campaigns are also crucial in educating consumers about the risks associated with Listeria and the importance of adhering to food safety practices.
By combining efforts at both the consumer and industry levels and through the proactive measures taken by public health authorities.
the risk of Listeria outbreaks can be significantly mitigated, ensuring a safer food supply for all.